Respiratory Disease
Hospital admissions for lung disease have risen three times faster than overall admissions in the past seven years, contributing significantly to NHS winter pressures.
Currently, a third of COPD patients are first diagnosed during hospital admission therefore over the next decade, the NHS Long-Term Plan will invest in improved treatment and early diagnosis, aiming to match or exceed international outcomes.
The NHS will enhance medication support, as improper use contributes to poor health outcomes, increased risk of exacerbations and hospital admission.
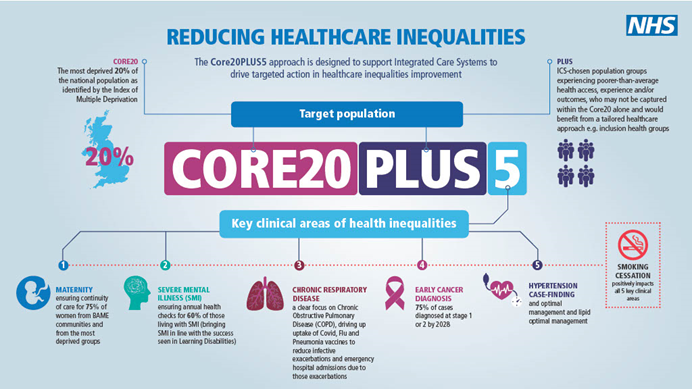
Additionally, the Core20PLUS5 initiative which targets health inequalities, prioritising chronic respiratory disease for accelerated improvement.


Identifying individuals with poor symptom control and those at risk of future asthma attacks allows for targeted care, improving quality of life for both patients and their families.
NHSI respiratory services are designed to support primary care practices in reviewing these high-risk patients, providing access to Specialist Respiratory Nurse.
- Patient identification and therapeutic review
- Clinical review – face-to-face or remote to ensure patients receive the most effective care
- Guideline level review using innovative technology
- HCP Education (incorporating RCGP accredited modules) and mentorship to build lasting expertise within practices
Identifying individuals with poor symptom control and those at risk of future asthma attacks allows for targeted care, improving quality of life for both patients and their families.
NHSI respiratory services are designed to support primary care practices in reviewing these high-risk patients, providing access to Specialist Respiratory Nurse.
- Practices referring less than a quarter of patients considered as ‘high risk’ in relation to the NRAD recommendations (Bloom ERS 4274)
- Inappropriate referrals contribute to long specialist waiting lists, sometimes up to a year, delaying effective management for patients with severe asthma


NSHI CSA services provide a Respiratory Specialist Nurse to work alongside the existing asthma clinical team, supporting the assessment and review of patients referred from primary to secondary care. This ensures accurate differentiation between difficult and severe asthma patients, allowing for management in line with established protocols.
Our service streamlines access to specialist care, allowing patients with severe asthma to be seen quickly, while those with difficult asthma are referred back to their primary care provider with an action plan aligned to national and local guidelines.
Many referrals to Specialist Asthma Centres lack comprehensive pre-assessment, making thorough evaluation essential for developing appropriate management plans.
COPD often coexists with other chronic conditions, making comorbidity a key challenge for the NHS. As one of the leading causes of respiratory mortality in the UK, COPD requires a holistic, shared care approach, with general practice playing a central role in long-term management.
The NHS Core20PLUS5 initiative prioritises chronic respiratory disease, by improving vaccine uptake to reduce exacerbations and emergency hospital admissions.
- Practices referring less than a quarter of patients considered as ‘high risk’ in relation to the NRAD recommendations (Bloom ERS 4274)
- Inappropriate referrals contribute to long specialist waiting lists, sometimes up to a year, delaying effective management for patients with severe asthma
NSHI implements services aligned with the NHS RightCare approach, supporting healthcare professionals in standardising clinical care, implementing national and local guidelines, and delivering cost-effective care that enhances patient outcomes. Our COPD review services provide practices with a Respiratory Specialist Nurse to deliver the following process.
- Patient identification and therapeutic review
- Clinical review of patients with COPD in line with NICE guidelines/GOLD Report/Locality guidelines
- F2F consultations incorporate diagnostics, which cannot be undertaken remotely
- Vitalograph copd-6 monitor used for all patients seen in clinic where last recorded FEV1 >6 months
- Spirometry as required
- Lifestyle counselling e.g. weight management, advice on stopping smoking (F2F & remote review)
- Education (incorporating RCGP accredited modules) and Nurse mentorship
- Review of inhaler technique during F2F and video consultations (it is not possible on telephone consultations)
Contact us |
|
|---|---|
| [email protected] | |
| Phone | 01760 721 279 |
